Great Books Vol 5: Contemporary and Wildly Useful Books Written by People I Know (at least on Twitter!)
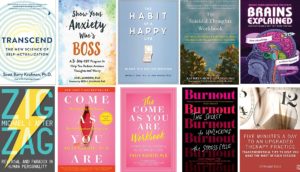
Transcend by Scott Barry Kaufman – This book is for everyone! It’s deeply humanistic and optimistic and transformational. If you thought you knew anything about Maslow’s “hierarchy of needs,” you should FOR SURE read this! It’ll both blow your mind and give you a great new metaphor for understanding human needs and actualization. Also, SBK is just this very cool, super authentic, and genuinely KIND human person. Oh, and he has the best podcast ever, too – The Psychology Podcast.
Show Your Anxiety Who’s Boss by Joel Minden – This is my favorite CBT book for clients. It’s easy to read, and the take-home message is simple and easy to remember (even though Joel knows I always roll my eyes at acronyms that are made to be cute, it turns out they are memorable!). One of my favorite things is how comprehensive it feels without turning into a long list of cognitive distortions. And I just really like the term “anxious fictions!”
The Habit of a Happy Life: 30 Days to a Positive Addiction by Jeff Zeig. Jeff has written a lot of books, and I like all of them that I’ve read (because the way he thinks, especially about therapy, is just brilliant), but they’re not all for a very broad audience. This one, however, would be very useful for many clinicians and clients alike. If you ever read Positive Addiction by William Glasser, I’d say this is like an update version – same great concept, newer research, and I like Jeff’s writing better than Glasser’s, too!
The Suicidal Thoughts Workbook by Kathryn Gordon – Is it weird to get really excited about a book on so heavy a topic? NO! Not for therapists, it’s not! Haven’t you lamented how few good resources there are for clients around suicide? This workbook is incredibly compassionate and thorough, gentle and practical. There’s no shying away from any difficult topics, and everything is handled with confidence in and grace for the reader. This is an indispensable resource for therapists, and I have no doubt it will be life-saving for clients.
Brains Explained by Micah & Alie Caldwell (and sort of by their cats). Look, I know I’m an intense nerd and so you won’t like all the books I like. But if you’re one of the HUGE number of therapists who is both really interested in neuro/brain stuff but sometimes also intimidated by neuro/brain stuff, you’re going to SWOON for this book! There’s definitely enough in there that’s genuinely relevant to clinical practice to make it worth the buy on its own – but be prepared to accidentally get swept up in all the rest of it, too. It’s just so…. accessible and hilarious! And the chapters are almost bite-sized. They’re like…dessert-sized. What more could you want? (Oh, they have a fun YouTube channel, too!)
ZigZag by Michael Apter – Michael is one of my most treasured mentors. If you’ve read any of the Reversal Theory blog posts, you have also benefitted from his brilliance! He’s also written several books, but this one is the newest introduction to RT and it’s really accessible. So many more people (including your clients and yourself!) will find this book somewhere between interestingly useful and life-changing, so give it a try!
Updated! Come As You Are by Emily Nagoski CAYA is my all time favorite book about sex!! Although it’s geared toward women, I almost always have men in relationships read it, too, especially if they’re in relationships with women. Emily is an incredible writer – she has a wild gift of taking really good, dense research and turning it into something both understandable and meaningful for the lay reader. Make sure you get the newest (revised & updated) version that was published in 2021, mostly because she says she likes it better.
Also, CAYA has a workbook! (In fact, two cool things about the workbook. One is that I am one of the people who helped review it for initial edits, which was super fun! The second is that I’m pretty sure my husband is the reason the book exists – when we first read CAYA in 2013, before Emily was crazy famous and busy, he just emailed her to ask if she had any of the exercises in PDF, so we didn’t have to mark up the actual book and we could have 2 of each of them. So, she made them into PDFs and emailed them. Then, she put them on her website. Then, this book became a thing!)
And, yes, I’m a Nagoski superfan, so Burnout: Unlocking the Secret to the Stress Cycle (by Emily & Amelia Nagoski) makes this list, too. Incredibly useful, especially for that subset of adult female clients who grew up learning that they had to always play support roles, even unto exhaustion (and maybe developed resentment, anxiety, or low self esteem as a result). Goes along nicely with the podcast The Feminist Survival Project 2020. Just a note – both the book and the podcast lean pretty heavily liberal, but as long as I have warned my conservative clients about that, it’s been ok.
Oh, and SURPRISE! I wrote a book, too! 😉 But you can’t have it until August!